Periodontists in Simi Valley
Schedule a Complimentary Consultation
Schedule Your Appointment Today Call Now: (805) 526-1000Unfortunately having a great smile doesn’t mean that your gums are healthy. In fact, many people with white, straight teeth suffer from periodontal disease, aka gum disease.
What is Periodontal Disease?
Periodontal disease is a general term for a group of dental diseases that have one main thing in common: loss of attachment of the gum, tissues, and bone to the teeth. Periodontal diseases are caused by bacterial infections and inflammation of gum tissue and in some cases the bone that surrounds and supports the teeth.
Most of these diseases are caused by bacteria and are asymptomatic in the early stages. However, they can harm the overall immune system and other body organs. Preventing gum disease development reduces the risk of heart disease, strokes, and dementia.
Gum disease is very easy to prevent, but once you have it, it is hard to treat it without complications. If you have early signs of periodontal disease (constant bleeding when you brush or floss your teeth, inflammation of the gums, bad taste and/or bad breath), don’t wait for your scheduled dental visit. Act as soon as possible in order to prevent more serious consequences. Our periodontists will help prevent, diagnose and create the highest quality treatment plan for your gum disease.
Symptoms of Periodontal Disease
Preventing tooth loss and damage to the soft tissue and jawbone, much less bad breath, requires good oral hygiene. But if you have the symptoms below, you should contact your dental office for a consultation. If left untreated, periodontal treatment may require dental implants or even bone grafts if it progresses far enough.
- Bad breath or a bad taste that lingers
- Red or swollen gums
- Gums that are tender or bleed easily
- Pain when chewing
- Loose teeth
- Sensitive teeth
- Receding gums or teeth that look longer
- Any change in the way your teeth fit together when you bite
- Any change in the fit of partial dentures
Periodontal Disease Risk Factors
The potential periodontitis risk factors include:
Smoking:
We all know that smoking is bad for our health. However, it also represents the most important risk factor for developing gum illnesses. Moreover, it can lower the chance of successful treatment.
Hormonal changes in women:
These factors can make the gums more sensitive, which enables gingivitis to occur more easily.
Pills:
Sometimes, over-the-counter medicines can reduce the saliva in the oral cavity, which has a protective influence for the mouth. If there is not enough saliva, the oral cavity may easily develop infections like gum illnesses.
Genetic predispositions:
Some patients can develop gum diseases more quickly than others.
Diabetes:
Patients who suffer from diabetes have a higher risk of getting infections, such as gum illnesses
Other diseases and their cures:
Illnesses like AIDS and its cures could have a negative impact on gum health, too. The same is valid for cancer
Understanding Gum Recession and Periodontal Disease
Gum or gingival recession occurs when gum tissue lowers exposing the teeth roots. When gums recede, the gaps are formed between the gum and teeth creating perfect conditions for bacteria growth and further complications. Gum recession makes your teeth more sensitive to cold, hot, and sugar and, in worse cases, provokes interdental bone loss. Gum recession is more typical for adults, however, teenagers can suffer from receding gums as well. Leaving gum recession untreated may cause tooth loss.
Why Do Your Gums Recede?
Gum recession can be caused by a variety of life habits, including:
- Aggressive flossing or brushing
- Teeth grinding
- Genetic disposition
- Trauma
- Poor oral hygiene
- Crooked teeth
- Low-quality dental care (badly fitted crowns, bridges, etc.)
- Smoking
- Piercing of tongue or lip
Symptoms of Gum Recession
Gum recession can flow without any signs. The biggest gravity of gum recession is its progressive nature. The symptoms may develop slowly over the years. However, there are some signs that can indicate that you have gum recession at the early stage:
- Teeth seem to be longer than usual
- Increased teeth sensitivity that doesn’t pass
- Teeth change their color
- You can see teeth roots
- Increased gaps between the teeth
- Red, inflamed or bleeding gums
- Bad breath or taste
- Tooth decay below the gum line
Gum Recession Treatment
In case of mild gum recession, nonradical measures can be taken such as a deep cleaning or scaling. For more severe cases, surgical treatment is the only way.
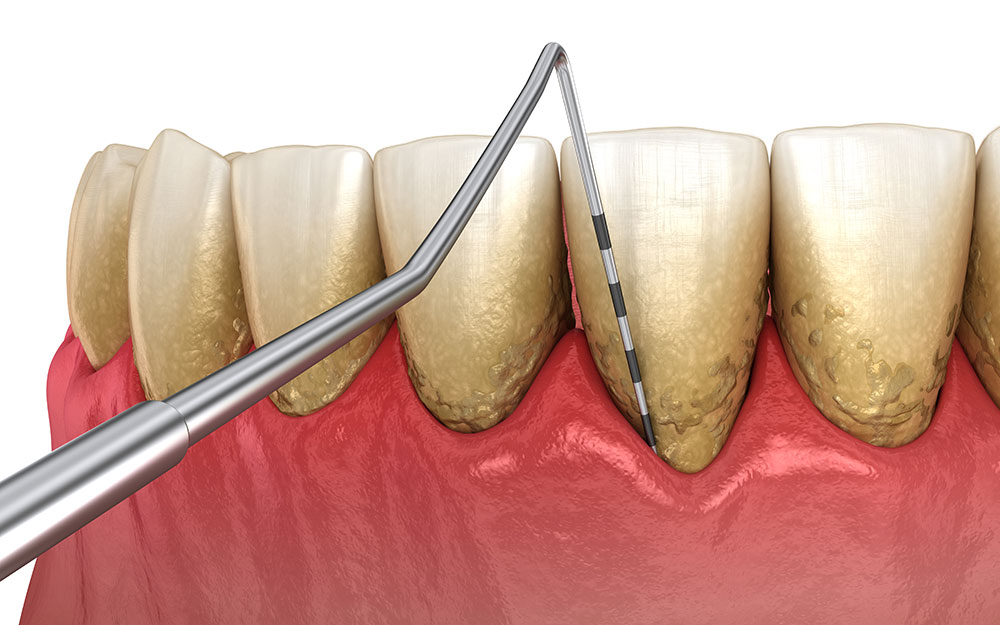
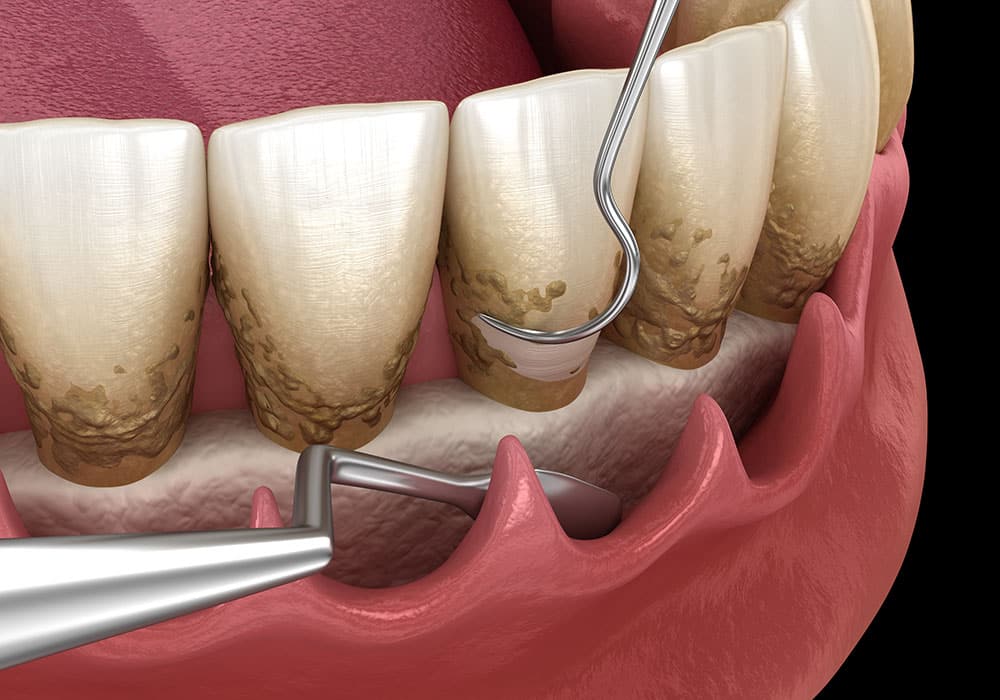
Deep Cleaning
Plaque and debris are usual teeth companions that create the so-called “pockets” between the teeth and gum. In normal cases, this situation doesn’t cause any harm, but if the gum disease has already started, your gums may become swollen and red. Deep cleaning is a less invasive procedure than gum surgery. It helps remove the places of bacteria accumulation and prevent further damage. During the deep cleaning or scaling, our specialists will remove debris and plaque from your teeth. Then, the exposed roots areas and gaps will be smoothed to prevent bacteria growth.
After Deep Cleaning
Straight after the procedure, be careful about how you brush and floss your teeth and what you eat. During the first days, your teeth can be very sensitive. Depending on the intensity of the procedure, the dentist may prescribe you some antibiotics or painkillers. Home dental care plays an essential role: your dentist can’t do it instead of you. After the cleaning, continue keeping proper oral hygiene. Brush and floss your teeth regularly, have balanced meals, and don’t forget to make follow-up visits to your dentist.
Soft Tissue Graft
A gum graft may be necessary to protect your teeth from more severe damage from gum recession. If your dentist says that you need gum surgery, don’t panic: it sounds scarier than it is. There are several types of grafts depending on the tissue type used for grafting:
Connective Tissue Grafts
During the procedure, a piece of skin is cut from a tissue flap from the upper part of your mouth (palate). Then, the connective tissue is grafted and stitched over the recessed area of the gum. Thus, all exposed roots become covered with grafted connective tissue. Usually, it takes around two weeks for wounds to heal and then the stitches can be removed.
Free Gingival Grafts
In this case, the tissue for grafting is taken from the palate directly and then attached to the recessed gum area. The procedure leaves the wound open and is usually more painful. A free gingival graft can be used for patients with thin gums when additional tissue is needed in order to enlarge the gums.
Pedicle Grafts
During this procedure, the tissue is taken from the gums around or near the damaged area. The pedicle is partially cut leaving one edge attached. Then, the gum is pulled over to cover the root and stitched. Pedicle graft can be done only when a patient has enough gum tissue around the affected tooth.
Soft Tissue Graft Aftercare
During the healing process (which usually lasts 4-8 weeks) soft tissues mature and bind the root surface and surrounding bone surface. The most important part of healing is the formation of new vessels that supply blood to the area. During the first weeks after the procedure you should eat soft foods and avoid brushing and flossing the gum line near the affected area. You may also be prescribed to rinse your mouth with a special rinse to block plaque creation during the healing process. Over-the-counter painkillers will help you feel more comfortable for a few days following gum surgery.
Pinhole Technique for Gum Recession
Traditionally, soft tissue graft was the only way to treat gum recession. In our dental office, we can offer you an alternative procedure with a less invasive option – a pinhole technique. The Pinhole technique doesn’t require incisions, stitches, donor tissue, or a long recovery time. During the procedure, a tiny hole is made in the affected gum. Through the hole, your emergency dentist will expand or loosen your gum tissue to make it cover an exposed part of the tooth root. Then, small collagen strips are used to help the gums stabilize. One of the biggest advantages of the pinhole technique is that a hole heals quickly – usually during one night. The procedure has a high success rate of achieving stable, long-lasting results and a beautiful smile.
Frequently Asked Questions
Can you get rid of periodontal gum disease?
Periodontal gum disease can be managed and its progression can be slowed through proper dental care, regular professional cleanings, and sometimes more advanced treatments, but complete elimination may not always be possible.
What are the four stages of periodontal disease?
The four stages of periodontal disease are gingivitis (mild inflammation of the gums), early periodontitis (bone loss begins), moderate periodontitis (increased bone loss), and advanced periodontitis (significant bone loss and potential tooth mobility).
Will I lose my teeth if I have periodontal disease?
In advanced stages of periodontal disease, tooth loss can occur if the supporting bone and tissues are severely damaged and cannot hold the teeth securely in place.
How long can teeth last with periodontitis?
The longevity of teeth with periodontitis varies widely depending on factors such as treatment, oral hygiene, overall health, and genetic predisposition, but timely and effective management can help teeth last longer.
Can you live a long life with periodontitis?
With appropriate management and oral care, it’s possible to lead a long life with periodontitis; however, the condition can impact overall health and quality of life if not properly addressed.
How long does it take for periodontitis to get serious?
The seriousness of periodontitis can progress differently in individuals, but early intervention is crucial; if left untreated, it can advance over several years, leading to significant damage to the teeth and supporting structures.
Will gums grow back after periodontitis?
While gums may not fully grow back after advanced periodontitis, proper treatment can help improve gum health, reduce inflammation, and prevent further progression of the disease, which may result in some tissue recovery.
Find Expert Treatment for Periodontal Disease at Elite Dentistry
At Elite Dentistry, we are dedicated to providing unparalleled care for individuals seeking expert treatment for periodontal disease. Our highly skilled team of dental professionals understands the significance of oral health and its impact on overall well-being. With state-of-the-art facilities and advanced techniques, our Simi Valley Dentists deliver comprehensive solutions tailored to each patient’s unique needs. Whether you require non-surgical interventions or advanced surgical procedures, our commitment to excellence ensures that you receive the highest quality of care. Trust Elite Dentistry to guide you towards a healthier smile and a brighter future, as we work together to combat periodontal disease and restore your oral health.